The U-M taps into smart devices, making medicine mobile.
The first commercial mobile phone was introduced to the American market in 1983. It was cumbersome and bulky, weighing about 30 ounces. It took 10 full hours to charge, but its convenience factor revolutionized communication. By 2015, more than 92 percent of American adults owned mobile phones, and 64 percent of those were smartphones.
Today, mobile devices have become much more than simple telephones. They have evolved into fully-fledged computers, complete with CPUs, RAM, graphics processors and GPS. And there’s an app for just about every use imaginable.
The University of Michigan Health System is at the forefront of this technological renaissance. With dozens of apps available as of spring 2016, faculty and students are using mobile technology to collect data, provide teaching tools, track symptoms — even monitor the progress of clinical trials.
“Mobile apps are probably our fastest-growing type of innovation [at UMHS],” says Connie Chang, managing director of Fast Forward Medical Innovation, or FFMI. To accommodate this boom, the Health System and the Medical School have developed a special path of excellence, or course of study, for first- and second-year students, called Innovation and Entrepreneurship, which launched earlier this year. It’s already the most popular path in the redesigned curriculum. Although not exclusive to app design and use, the pathway allows greater focus on mobile device integration in the medical world.
Chang and her colleagues at FFMI also work closely with the U-M Office of Technology Transfer, or OTT, which has spearheaded efforts to streamline app development and steward potential app creators through the sometimes intimidating process. “The goal is to help bridge the gap between the university and industry,” says Drew Bennett, associate director of software licensing.
Other areas at the university are able to lend additional expertise, including the Medical School Information Services department, or MSIS, and the Center for Health Communications Research.
Most of the apps U-M has produced are available for little to no cost with easy-to-use layouts and scientifically-backed data. This integration of technology, real-time information and personalization is one of the many ways U-M is helping people maintain their health and well-being, no matter where they are.
Read on for some examples of U-M-made apps.

MyBreastCancerAlly
MyBreastCancerAlly helps patients at any stage of diagnosis organize, understand and prepare for treatment. It employs a “targeted education” model to deliver specific information related to the user and can help with the management of appointment times, medication reminders and exercise routines. Michael Sabel, M.D., the William W. Coon Collegiate Professor of Surgical Oncology and chief of the Division of Surgical Oncology, conceptualized and created the app with input from surgeons, oncologists, nurses and additional staff, who helped customize the user experience. The Center for Health Communications Research provided developmental help. Currently, the app is only available for patients at the U-M Comprehensive Cancer Center.
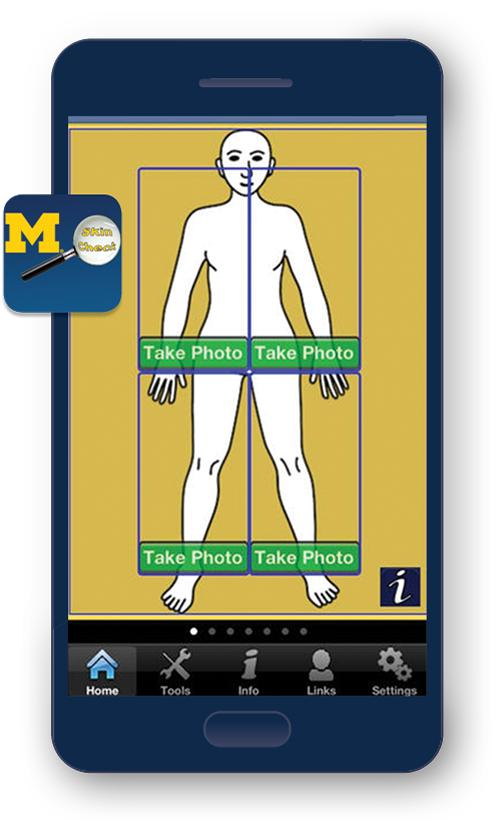
UMSkinCheck
UMSkinCheck has a simple interface that teaches users how to conduct thorough self-examinations for melanoma. Along with the guide, users can take photos of suspicious or problem areas to compare and/or track them. Michael Sabel, M.D., the William W. Coon Collegiate Professor of Surgical Oncology and chief of the Division of Surgical Oncology, provided guidance, in addition to the divisions of surgical oncology and cutaneous oncology (dermatology), which offered medical tools and information. MSIS helped deploy the app.
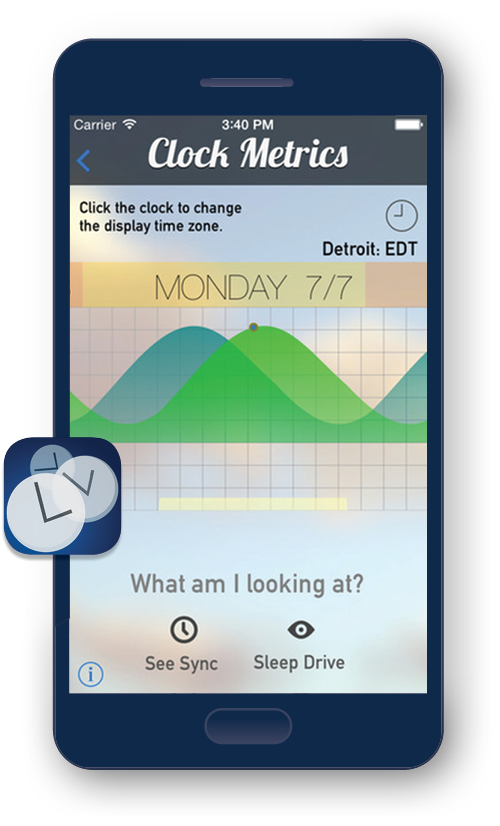
Entrain
Entrain uses mathematical data to provide recommended lighting schedules for travelers experiencing jetlag. Since launching in 2014, thousands of users have followed customized “light” and “dark” exposure hours to readjust their body to the local time. In 2016, information submitted by Entrain users was included in a study of global sleeping habits, marking a breakthrough achievement for data-gathering through apps. Its model is also influential for other sleep researchers, like Cathy Goldstein, M.D., assistant professor of neurology, who is developing a way to monitor sleep times and duration. Olivia Walch, a Ph.D. candidate in the Department of Mathematics; Daniel Forger, Ph.D., a professor of mathematics and of computational medicine and bioinformatics; and Kirill Serkh, a U-M graduate who is now a Ph.D. candidate at Yale University, worked with the OTT to deploy the app, which was developed and designed by Walch.
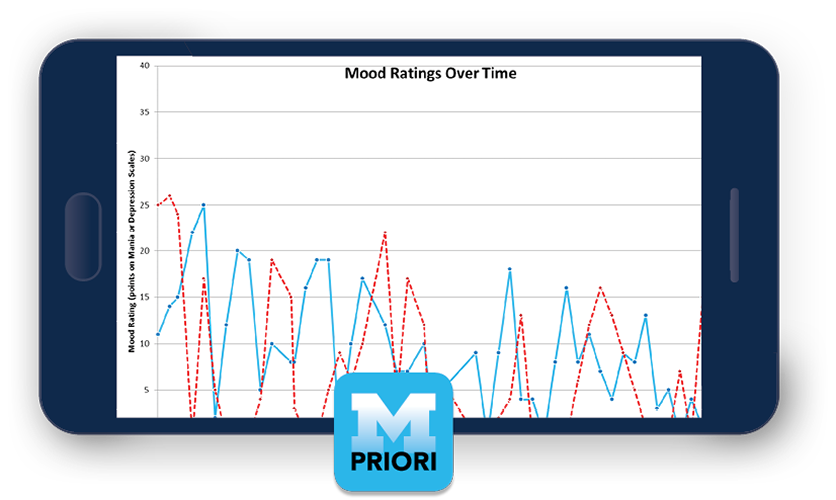
PRIORI
PRIORI — Predicting Individual Outcomes for Rapid Intervention — detects subtle voice variations to predict mood changes in people with bipolar and mood disorders. Available on designated phones as part of a research study, it runs securely in the background of a mobile device, monitoring outgoing calls (only the user’s side is recorded). PRIORI was developed by the College of Engineering (Emily Mower Provost, Ph.D., assistant professor of engineering and computer science) and the Medical School (Melvin McInnis, M.D., the Thomas B. and Nancy Upjohn Professor of Bipolar Research and Depression and director of the Prechter Bipolar Research Fund), with help from the OTT, the Michigan Institute for Clinical and Health Research and the Michigan Translational Research and Commercialization Program.
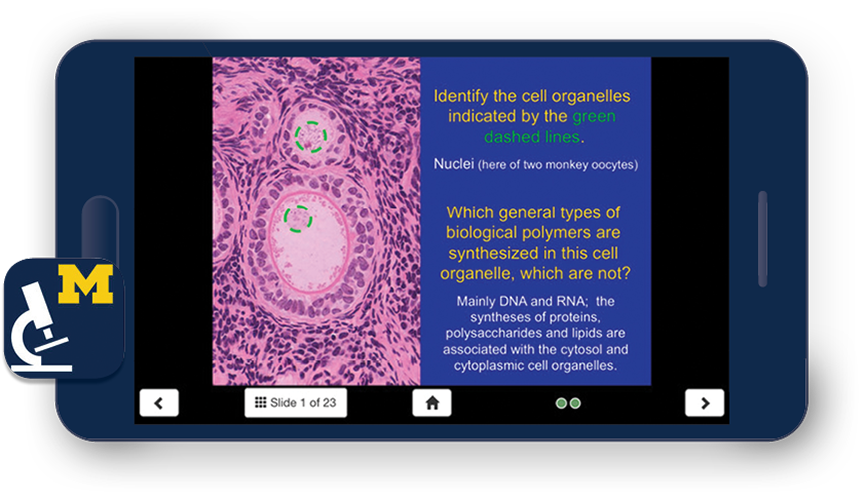
SecondLook Histology Series
One of the university’s first publicly available apps, SecondLook Histology has helped medical professionals and students review and retain histology information since 2012. The award-winning app, created by Michael Hortsch, Ph.D., associate professor of cell and developmental biology and of learning health sciences, provides self-evaluation tools based on information gathered from various faculty, graduate, medical and dental students, and has been downloaded over 15,000 times. Based on its success, the SecondLook series has moved on to the subjects of neuroanatomy and musculoskeletal anatomy. All SecondLook apps are available free to U-M faculty, students and staff, and were developed with help from MSIS and the OTT.

ManageHF
ManageHF was released in summer 2014 to help patients navigate and learn about heart failure, a chronic condition that impacts blood flow into and out of the heart. Currently, almost 5 million people are living with heart failure in the U.S. Michael Dorsch, Pharm.D., a clinical associate professor in the College of Pharmacy, and Todd Michael Koelling, M.D., professor of internal medicine, created ManageHF to make knowledge about heart failure accessible. Available to current patients at U-M, ManageHF has helped hundreds of users monitor and manage their symptoms. Dorsch worked with the OTT to launch the app and contributed his own finances to expedite the development process.
MyGIHealth
MyGIHealth helps users manage and understand their gastroenterological problems by providing a “snapshot of a person’s GI illness experience [and] integrating the information gathered into a written history,” says William D. Chey, M.D. (Fellowship 1993), co-creator of the app and professor of internal medicine. That history can be downloaded by a health care professional and added to the user’s medical records. The app is a collaborative effort between Chey, also the director of the U-M GI Physiology Laboratory and of Medical Services for the Michigan Bowel Control Program; Brennan Spiegal, M.D., director of Cedars-Sinai Health Services Research; and Chris Almario, M.D., a gastroenterologist at Cedars-Sinai Medical Center. The U-M Center for Health Communications Research played a key role in the app’s creation.
miAFib
In 2015, miAFib was launched along with a research study to collect information on the effects and symptoms of atrial fibrillation — the most common major arrhythmia in the United States — in patients with a confirmed diagnosis. The app is combined with sensors to retrieve up-to-the-minute, accurate data, which is then communicated to the patients’ doctors and health care professionals. The purpose of the study is to follow daily fluctuations in symptoms, which are difficult to quantify in a single doctor’s appointment, to better target and treat individual patient needs. miAFib, created by Hamid Ghanbari, M.D. (Fellowship 2011), clinical lecturer of internal medicine, is a cross-disciplinary collaboration between the College of Engineering and the departments of internal medicine and psychology at the Medical School. The OTT provided developmental help and guidance. Currently, it is only available to U-M patients participating in the research study.

